Post-Exposure Management of Multidrug-Resistant Tuberculosis Contacts: Evidence-Based Recommendations
The Harvard Medical School Center for Global Health Delivery–Dubai celebrated its inaugural symposium on Sunday, October 25, 2015 at the Mohammed Bin Rashid Academic Medical Center in Dubai Healthcare City. At the launch, the Center distributed a policy brief, “Post-Exposure Management of Multidrug-Resistant Tuberculosis Contacts: Evidence-Based Recommendations,” which was written by Sentinel Project members.
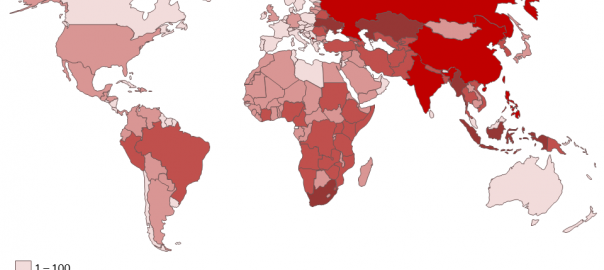
The principles and recommendations outlined in this policy brief were developed by a global panel of 51 tuberculosis practitioners from 33 cities in 19 countries who gathered at the Harvard Medical School Center for Global Health Delivery–Dubai on April 12 and 13, 2015. This global consultation provided a forum for TB practitioners to synthesize evidence and produce practical guidance for the management of children and adults who are household contacts of patients with DR-TB. Following the meetings and a review of published and unpublished evidence, the panel arrived at a set of seven principles summarized in this policy brief, along with the process employed to produce them.